EDC-MASLD is an EU-funded project focused on exploring the role of Endocrine-Disrupting Chemicals (EDCs) in the progression of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). With MASLD affecting 25% of the general population, it’s crucial to understand all contributing factors for effective prevention and intervention.
EDC-MASLD investigates the impact of EDCs on the internal exposome across various dimensions (metabolome, gut microbiome, epigenome, proteome, immunome), emphasizing prospective studies during the transition to progressive MASLD stages. Leveraging the rich European NAFLD Registry with over 9,000 characterized patients, the consortium examines the intricate interplay between EDC exposure, sex, genotype, diet, socioeconomic, and lifestyle factors.
The EDC-MASLD consortium has diverse and complementary expertise in the domains of hepatology, endocrinology, toxicology, exposome research, metabolomics, systems biology, environmental economics, and communications & technology research, with respective PIs being global leaders in their fields. Taken together, EDC-MASLD will significantly contribute to the actions centred on identification and mechanistic assessment of impact of EDCs, strategies to monitor and reduce exposure, and regulatory actions that could better protect human and environmental health.
Objectives / aims
- To characterise the impact of environmental exposure to EDCs on the internal exposome (metabolome, gut microbiome, epigenome, proteome, immunome) and degree of liver damage in MASLD in prospective study settings.
- To understand the mechanisms of hepatic injury and resolution due to exposures to EDCs.
- To develop and implement an integrative systems biology and screening platform for the studies of EDCs in MASLD.
- To identify and evaluate pathways to impact, targeting key stakeholders and citizens.
Planned studies and project outcomes
- The project will perform multi-omics / exposomics clinical studies, with a focus on the period of transition to progressive stages of MASLD, investigating chemical exposure, mixture effects, interaction with diet, medication, sexual dimorphism, infections, vaccinations, stress, and socioeconomic factors, etc..
- EDC exposure studies will be performed in murine models of MASLD, zebrafish models, and 2D/3D in vitro models.
- Multiple computational (e.g., AOPs, genome-scale metabolic models) and experimental (in vitro, in vivo) tools will be set up for the assessment of the impact of EDCs and their mixtures, in the context of MASLD, generalisable to other applications.
- We will investigate MASLD patients’ socioeconomic and cultural profiles and lifestyles and assess public support to eliminate EDCs from European markets in support of relevant EU legislation.
Work package structure
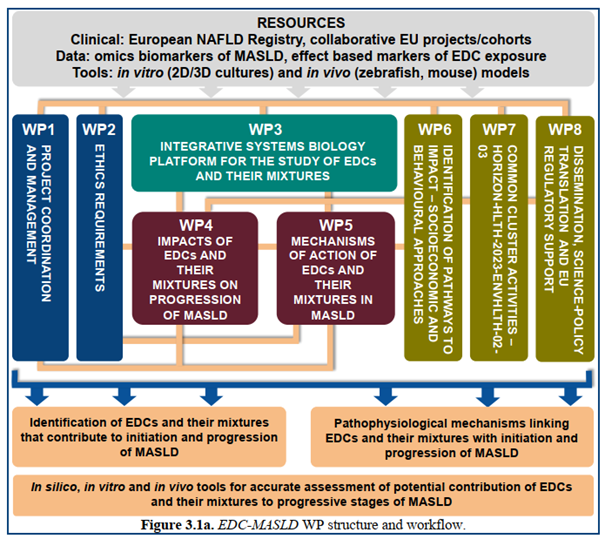
Work packages
- WP1: Project coordination and management, lead by Örebro University
- WP2: Ethics requirements, leady by Saarland University
- WP3: Integrative systems biology platform for the study of EDCs and their mixtures, lead by Örebro University
- WP4: Impacts of EDCs and their mixtures on progression of MASLD, lead by University of Turin
- WP5: Mechanisms of action of EDCs and their mixtures in MASLD, lead by Utrecht University
- WP6: Identification of pathways to impact – socioeconomic and behavioural approaches, lead by Vrije Universiteit Amsterdam
- WP7: Common cluster activities HORIZON-HLTH-2023-ENVHTLH-02-03, lead by Örebro University
- WP8: Dissemination, science-policy translation and EU regulatory support, lead by empirica
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)
MASLD is the condition of excessive accumulation of liver fat unrelated to alcohol intake, ranging from simple fatty infiltration (a benign condition called steatotic liver disease) to metabolic dysfunction–associated steatohepatitis (MASH), defined as the presence of fat leading to lipotoxicity and inflammatory damage to hepatocytes.
With a 25% prevalence in the general population, MASLD is currently the most common liver disease in Western diet-consuming countries, paralleling the increase in obesity and type 2 diabetes (T2D). 25% of patients with MASLD may have MASH, the second leading cause of liver disease in adults scheduled for liver transplantation in the USA[1], posing a major healthcare and economic burden.
It is difficult to distinguish MASLD from alcoholic hepatitis, for which alcohol consumption must be ruled out as cause. While hyperlipidaemia, obesity and insulin resistance are the major risk factors for MASLD and contribute to its rising prevalence, some factors are still unclear.
Endocrine Disrupting Chemicals (EDCs)
The endocrine system is a network of glands and organs that produce hormones that control many biological processes like growth, fertility, and reproduction.
Endocrine-disrupting chemicals (EDCs) are natural or human-made chemicals that may mimic, block, or interfere with the body’s endocrine system. EDCs can come from many different sources and there are many ways people are exposed to these chemicals: breathing, eating, drinking, but also through skin absorption.[2]
Some EDCs act like “hormone mimics”, acting similarly as naturally occuring hormones, while other EDCs can block the action of the natural hormones. Other chemicals can alter the ability of the body to synthesise, release, or eliminate hormones. Continuous exposure to EDCs can therefore disrupt the delicate balance of the endocrine system.
The potential role of EDCs in MASLD
EDC exposure in early life might reprogram hepatic lipid homeostasis towards a metabolic ‘set point’ that promotes MASLD. Growing evidence suggests that exposure to EDCs can induce initiation and / or progression of MASLD, either directly or by exacerbating the effects of a high-fat diet, genetics and / or lifestyle factors[3]. EDCs can interfere with metabolic processes, although the mechanisms of action are still poorly understood. While hyperlipidaemia, obesity and insulin resistance are the major risk factors for MASLD and contribute to its rising prevalence, exposure to EDCs may act as a ‘second hit’ in the progression of MASLD, advancing from earlier stages of liver damage to more advanced stages such as MASH and cirrhosis.[4],[5]
Alternatively, exposures may even represent the ‘first hit’ which compromises the liver’s protective responses against over-nutrition, predisposing it to steatohepatitis following a subsequent ‘hit’ from a hypercaloric diet[6]. Notably, recent genetic data (from a genome-wide association study) provides evidence of nuclear receptor PPARG acting as a risk factor for MASLD[7].
EDCs can have both direct and indirect impacts on the host metabolism. The direct impact is seen by the capability of EDCs to interact with hormone receptors[8]. In early-life, EDC exposures can impact the epigenome, altering DNA methylation and / or histone modifications to affect metabolic reprogramming via altered expression of hepatic lipid pathway genes[9], [10].
[1] Satapathy SK, Sanyal AJ. Epidemiology and Natural History of Nonalcoholic Fatty Liver Disease. Semin Liver Dis. 2015;35(3):221-235.
[2] https://www.endocrine.org/patient-engagement/endocrine-library/edcs
[3] Foulds CE, Trevino LS, York B, Walker CL. Endocrine-disrupting chemicals and fatty liver disease. Nat Rev Endocrinol. 2017;13(8):445-457.
[4] Trevino LS, Katz TA. Endocrine Disruptors and Developmental Origins of Nonalcoholic Fatty Liver Disease. Endocrinology. 2018;159(1):20-31.
[5] Wahlang B, Jin J, Beier JI, et al. Mechanisms of Environmental Contributions to Fatty Liver Disease. Curr Environ Health Rep. 2019;6(3):80-94.
[6] Ibid.
[7] Vujkovic M, Ramdas S, Lorenz KM, et al. A multiancestry genome-wide association study of unexplained chronic ALT elevation as a proxy for nonalcoholic fatty liver disease with histological and radiological validation. Nat Genet. 2022;54(6):761-771.
[8] La Merrill MA, Vandenberg LN, Smith MT, et al. Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification. Nat Rev Endocrinol. 2020;16(1):45-57.
[9] Foulds CE, Trevino LS, York B, Walker CL. Endocrine-disrupting chemicals and fatty liver disease. Nat Rev Endocrinol. 2017;13(8):445-457.
[10] Robles-Matos N, Artis T, Simmons RA, Bartolomei MS. Environmental Exposure to Endocrine Disrupting Chemicals Influences Genomic Imprinting, Growth, and Metabolism. Genes (Basel). 2021;12(8).